What they’re trained for
Biomedical engineers at UNC-Chapel Hill and NC State respond to COVID-19 by teaming to speed the development of an emergency ventilator
Biomedical engineering student Kathlyne Bautista always knew that her coursework and training would set her on a path to make a life-changing difference for people. But before the coronavirus pandemic, she didn’t realize just how soon that opportunity would arrive.
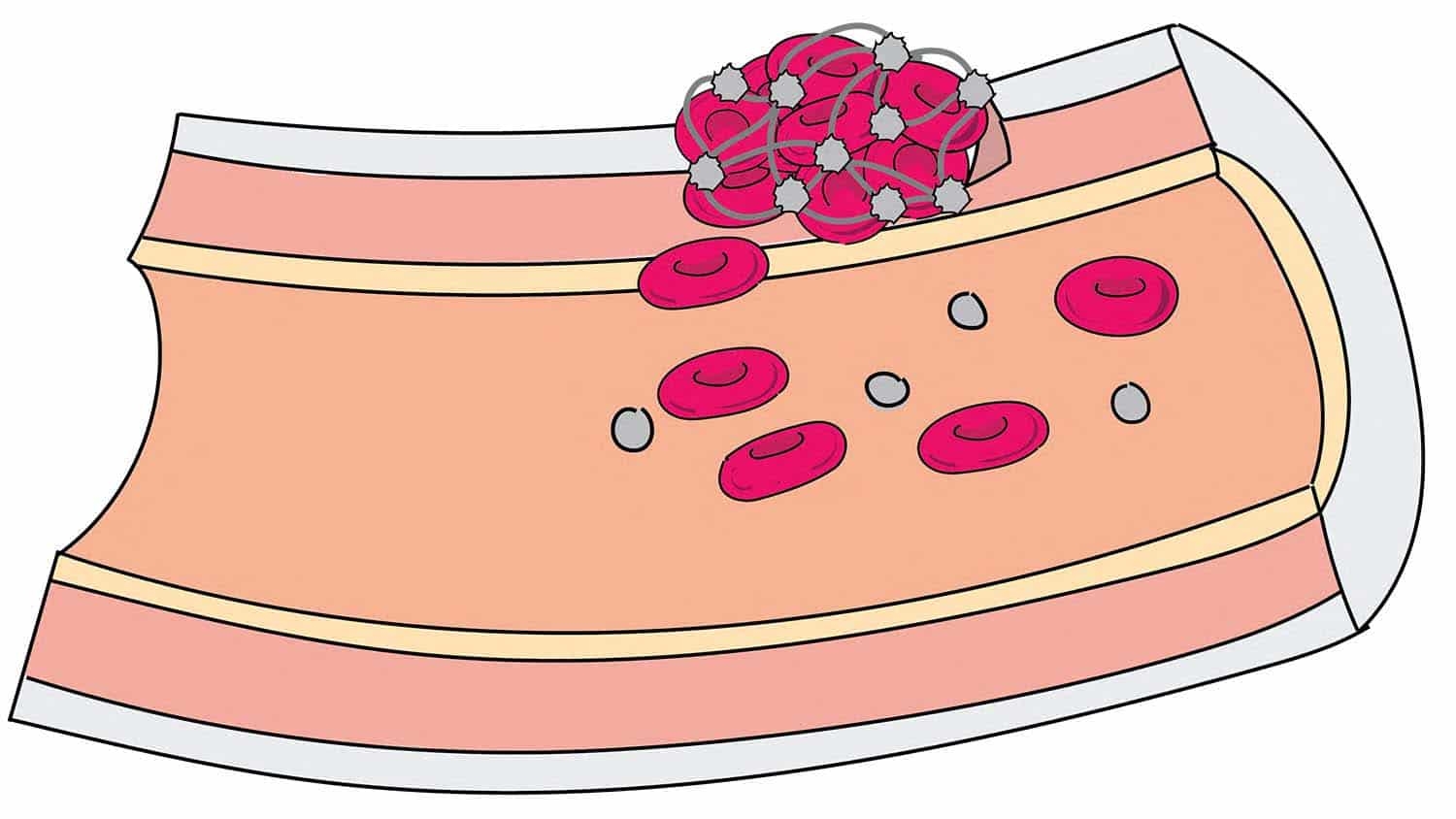
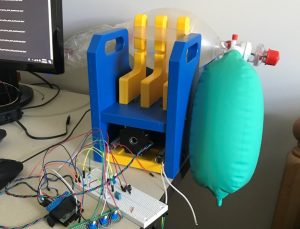
Bautista is part of the Carolina Respiratory Emergency – Ventilator (CaRE-Vent) team led by Dr. Yueh Lee, MD, an associate professor at the University of North Carolina at Chapel Hill. His research team is sprinting to design and prototype an open-source ventilator in a matter of weeks that has the potential to help fill a critical equipment gap caused by a projected spike in COVID-19 patients. The group is designing the ventilator so that it could be manufactured quickly and inexpensively – at less than $1,000 and with only six hours of skilled labor per unit.
And even in the best-case scenario – where the COVID-19 curve flattens to the point that the device is never needed for patients – the team’s efforts are advancing knowledge in the biomedical design community about the best way to create emergency ventilators in the future.
“I’m very grateful to have the opportunity to potentially save lives. As an engineer, it’s what you are training for,” said Bautista, an undergraduate student in the UNC/NC State Joint Department of Biomedical Engineering who has been creating mechanical designs for the ventilator. “You learn all this math and take all these classes, but in the end, you want to do something that’s worthwhile.”
The biomedical engineering department, which blends the medical knowledge of researchers at UNC-Chapel Hill and engineering expertise of those at NC State University, has bridged faculty and students from both institutions to work quickly on the ventilator. Other schools and departments at both universities, including the UNC School of Medicine and NC State Department of Mechanical and Aerospace Engineering, have joined the effort, along with UNC Health and multiple industry partners, including Toshiba Global Commerce Solutions headquartered in Research Triangle Park and ShopBot Tools headquartered in Durham. They share a common charge: figuring out how to develop an emergency ventilator in a time crunch.
“This is what biomedical engineers are trained for – being given a problem in medicine and bringing engineering tools in to solve that problem,” said Paul Dayton, interim chair of the biomedical engineering department and William R. Kenan Jr. Distinguished Professor. “The design process and prototyping are all part of our curriculum. This has been a real-world – and much more urgent – implementation of what our students are trained to do.”
Dayton says that he’s been putting together groups that can collaborate and solve important coronavirus-related problems fast. The CaRE-Vent team headed by Lee, an associate professor of radiology at the UNC School of Medicine and adjunct assistant professor of physics, astronomy and biomedical engineering, is one that Dayton helped forge by connecting complementary talents from UNC-Chapel Hill and NC State.
“The team led by Yueh Lee got together and has been moving full-speed ahead toward developing prototypes,” Dayton said.
It turns out that Lee’s team didn’t have to start completely from scratch. Its new prototype was inspired by a device designed over a decade ago by Richard Feins, MD, a thoracic surgeon and retired professor who led the UNC School of Medicine’s Cardiothoracic Simulation Lab. It’s here where the mechanism – which employs a resuscitation bag and windshield-wiper motor – helped create a more realistic training environment for surgical students by reanimating pig hearts and lungs. Lee also used the mechanism for his imaging research at Carolina.
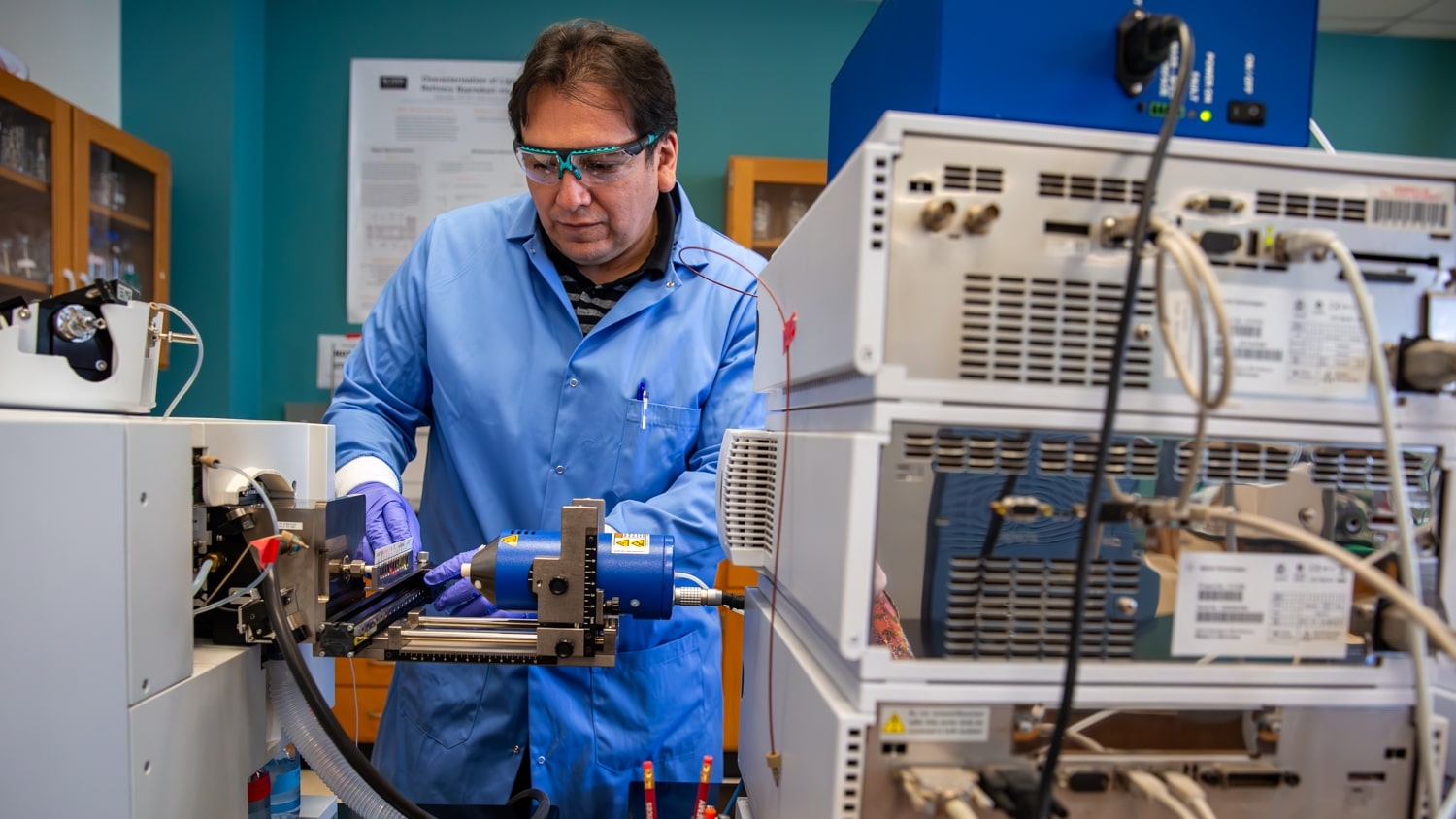
“We’ve had this unit for quite a while sitting in the lab,” said Lee, who cites Nabil Khan, a prototype and design engineer with FastTraCS of the North Carolina Translational and Clinical Sciences (NC TraCS) Institute, as his project co-lead. “We knew we already had a prototype that could ventilate a lung and said, ‘Why don’t we start from there?’ We were inspired by that as a starting point.”
As work on the ventilator progressed, members of the NC TraCS team provided expertise. “It has been rewarding to apply our knowledge as part of the CaRE-Vent team to help move such a vital project forward,” said Amanda Wood, TraCS regulatory specialist. “NC TraCS provides knowledge and experience that can have a real impact on final prototype designs, and we were excited to provide valuable guidance to improve this device.”
For Lee and his team, next steps happen by the minute. “We want to have something that we can release as open source so others can manufacture it to their own local standards – and we want to release that as soon as possible,” Lee said.
Innovating faster together
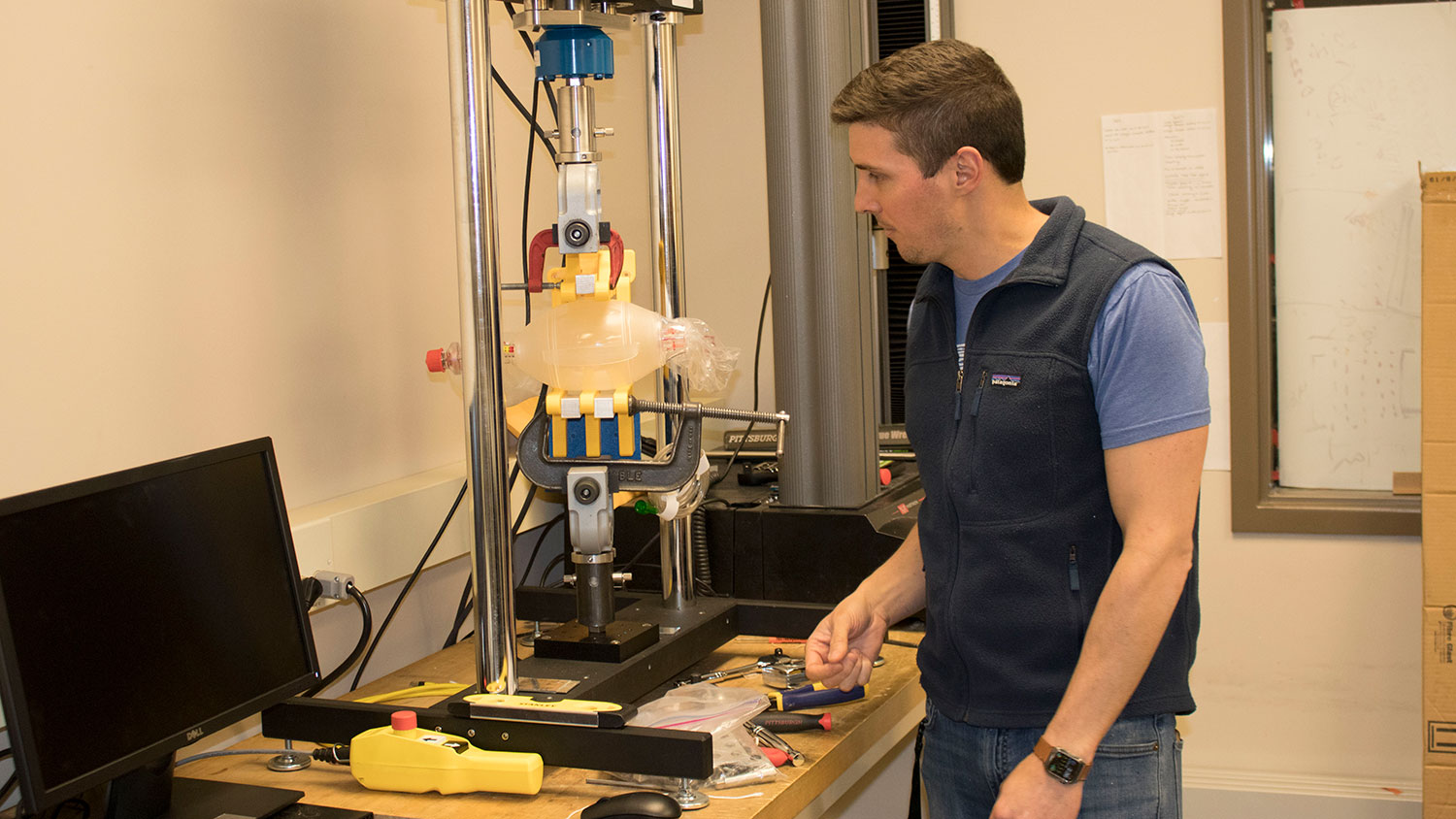
Within two weeks of launching the CaRE-Vent project, the team was already testing and validating a ventilator prototype. All members of the group say they would not have progressed so far so quickly if not for cross-university collaboration. Lee’s group is working closely with a team led by Landon Grace, an assistant professor of mechanical and aerospace engineering at NC State.
“The CaRE-Vent project is a perfect example of collaboration. There are so many different components of the project that one group would just not have the expertise to do on its own,” said Grace. “Because we need to move so fast, you have to find people to join the team that already have the expertise, know what they’re doing and can contribute immediately. And that’s what we’ve been able to do. It’s been incredible.”
Knowing their individual strengths, UNC-Chapel Hill and NC State rely on each other and expertly perform their respective parts. Carolina brings the medical expertise drawn from physicians and researchers at the UNC School of Medicine, plus faculty and students with advanced knowledge in 3D printing, laser cutting, CNC work and rapid prototyping capabilities. NC State is working through the mechanical design, fatigue testing, and the creation and testing of a positive end-expiratory pressure (PEEP) valve for the ventilator.
“The NC State team gives us the confidence that if we need a higher level of engineering, or access to a very specific engineering tool that UNC doesn’t have, it’s a quick phone call,” said Lee. “With a background as a mechanical engineer, I know if I need to walk through an engineering principle that I want to verify or validate, it’s a quick touchstone to walk through that with Landon’s team.”
Adds Grace, “The sense of urgency is something we don’t really ever see, and I have been amazed as to how it’s brought out the best in every member of the team. The communication, collaboration and the speed at which it’s happening is something I would not have predicted.”
Dayton says everyone involved is rallying together to do something bigger than they could do by themselves.
“The team is working really hard because they think they can make a difference and potentially save lives, and that’s been the spirit of everyone working together,” said Dayton. “We’re going to do our best job as fast as we can because it can make an immediate difference. It’s been a really positive environment.”
Lee’s team received advice and design suggestions from other faculty at the UNC School of Medicine, including Jason Akulian, MD, assistant professor of medicine and director of interventional pulmonology; and Thomas Bice, MD, assistant professor of medicine and medical director of adult respiratory therapy. Equipment borrowed from his research collaborators, David Fleischman, MD, an assistant professor of ophthalmology, and Jennifer Goralski, MD, an assistant professor of medicine and pediatrics and member of the Marsico Lung Institute, helped move the design process forward. And experts from UNC Health, including Thomas Devlin, a respiratory therapy clinical specialist, and Tracy Roberts-Brazil, a clinical educator in respiratory therapy, also provided critical insights to the CaRE-Vent group.
Collaboration with innovative industry partners, like Toshiba Global Commerce Solutions, also provides real-world expertise in manufacturing processes and efficiencies to help inform the design. “We’re used to working with some of the most successful retailers in the world, now helping them operate and deliver essential services to the communities in which they operate,” said Fredrik Carlegren, vice president of marketing. “We are thrilled to collaborate with UNC-Chapel Hill and NC State teams to build prototypes to support their design and ultimately do good for our community and those in need.”
Real-life learning

To round out the CaRE-Vent team, Lee added several UNC BME students, including Bautista and graduate students Sang Chung and Thomas Kierski. They’re all learning in a way that isn’t possible in a classroom.
Chung is testing how the system performs, including collecting data and reporting troubleshooting errors that come up during testing.
“It gives me a sense of purpose and urgency, and there is nothing else I would rather be doing now,” Chung said.
Kierski, who is tackling the programming and integration side of the project adds, “It’s been an eye-opening experience.”
The students are embracing the project as a chance to get hands-on training with their faculty mentors on an urgent, ever-shifting project.
“From an engineering perspective, this is it. This is what we live for – solving problems when the stakes are high and the problems are difficult. It’s been a learning experience for my team,” said Grace. “You can’t duplicate it in a classroom or a lab. That’s one of the underlying things that’s happening that is incredibly valuable outside of the work itself – the lessons the students are learning.”
This is the kind of situation, Dayton says, that biomedical engineering students are prepared to tackle.
“Part of our BME educational experience is the design process, which is exactly what we’re doing here,” said Dayton. “You’re presented with a problem, you talk about ways to solve it, you come up with prototypes, you test your prototypes, and you move your design forward.”
For Lee, the ability to work across disciplines with faculty colleagues and students has been critical.
“We are very fortunate, and UNC is unique because we have very few silos,” he said. “We have a very collaborative culture.”
- Categories: